Advancements in understanding of Alzheimer's Disease
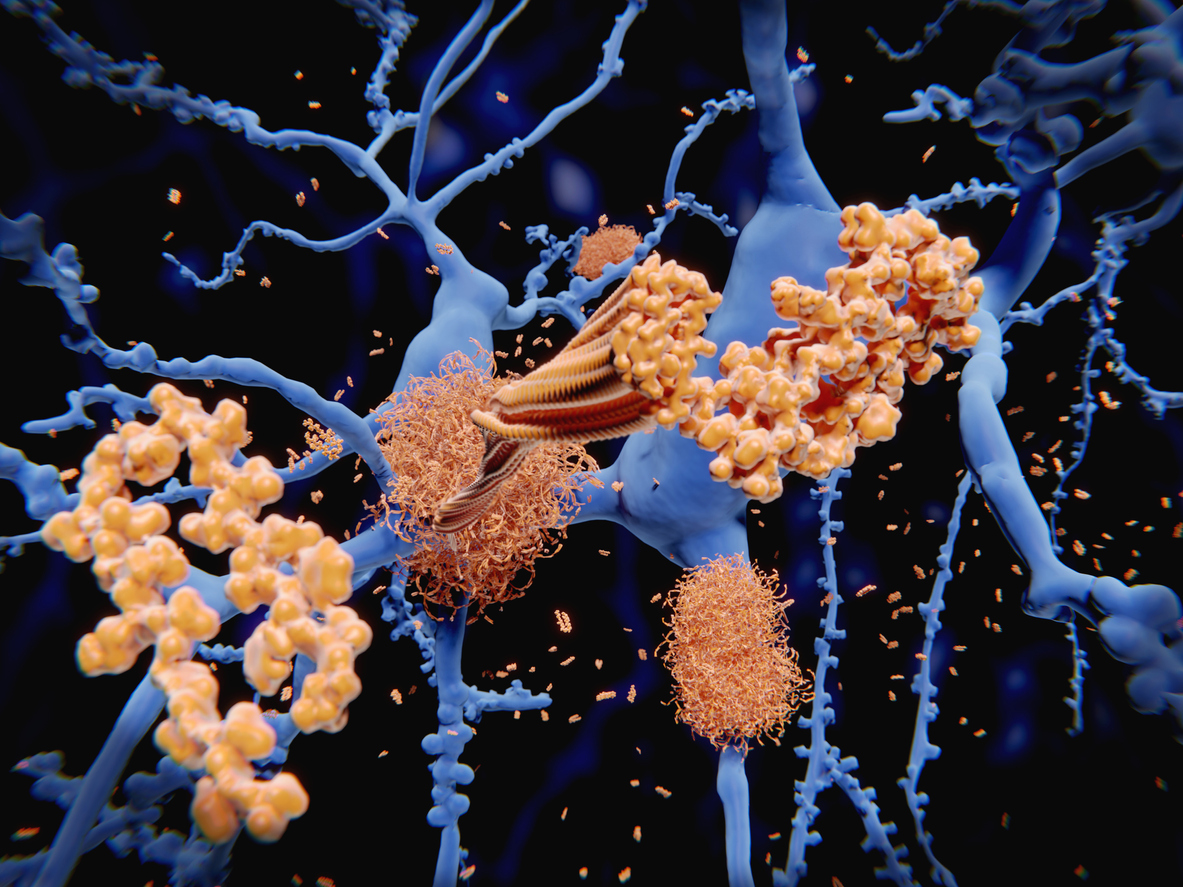
Video: How Alzheimer's Changes the Brain
The scientific community’s understanding of the pathological processes defining Alzheimer’s disease is currently experiencing a rapid and welcome transformation due to the advent of easily accessible blood-based biological markers of disease (biomarkers). The capability to effectively measure biomarkers across all stages of Alzheimer’s disease provides new opportunities for both the clinician and patient to enable greater well-being, planning and preparation throughout the disease continuum.
An understanding of the science behind these advances can help people take control of their journey and create hope for today.
The revolution of blood-based biomarkers
Compared to current methods for determining the likelihood of AD, blood-based biomarker tests are less expensive, less invasive, and are more broadly accessible because they do not require highly specialized instruments. In particular, pTau217 is a tau protein found in blood that is considered to have the highest accuracy in predicting a diagnosis of AD. This is supported by longitudinal studies where pTau217 predicted future progression from normal cognition and mild cognitive impairment to AD and in post-mortem studies where pTau217 differentiated AD from other types of dementia.
ALZpath has established a robust and scalable plasma-based ultra-sensitive assay, branded ALZpathDx, utilizing a proprietary monoclonal pTau217 antibody and peptide calibrator. This ultra-sensitive blood-based ELISA assay has been developed on the semi-automated single-molecule array Simoa® platform. ALZpathDx has been launched for clinical use as laboratory-developed test (LDT). Evaluation in independent clinical cohorts with multiple co-morbidities is currently being established to advance to an in-vitro diagnostic (IVD). This pTau217 Simoa® assay is a fit-for-purpose validated assay now available for commercial use.
The introduction and widespread use of accurate and universally available blood-based biomarkers will revolutionize early diagnosis. It will enable doctors, patients and their families to make more informed decisions much earlier in the disease process.
The evolution of an Alzheimer’s disease diagnosis
In the past 45 years, cognitive testing has been the main method used to diagnose Alzheimer’s disease. However, relying solely on cognitive testing has limitations because people only show cognitive symptoms after significant changes have already happened in the brain. Detecting the disease earlier is important for effective interventions. Before the early 2000s, the only definitive way to confirm if a patient had Alzheimer’s disease was through autopsy after death. Fortunately, over the past 20 years, brain imaging techniques like PET, CT, and MRI have been developed to assist in diagnosing Alzheimer’s disease with more certainty. However, these brain scans, especially the amyloid PET scan, are expensive, expose patients to radiation, and are not accessible for many patients. These drawbacks make imaging diagnostic procedures less useful for both patients and doctors.
To overcome these challenges, researchers have turned to biomarkers in peripheral fluids. In the last decade, cerebrospinal fluid (CSF) biomarker assessments have become an important additional diagnostic tool alongside bioimaging. These assessments involve examining CSF for changes in amyloid plaques and tau proteins, which reflect biochemical changes in Alzheimer’s disease progression. However, obtaining CSF through a lumbar puncture is an invasive procedure that requires specialized practitioners in a hospital setting. Now, we have the ability to detect biomarkers in blood, which is easily accessible and performs just as well as CSF. Detecting biomarkers in blood is considered the future of diagnosing Alzheimer’s disease because it is easily accessible, affordable, and can be scaled up to serve large numbers of patients.
Alois Alzheimer publicly presents his finding on pre-senile dementia on November 3rd, 1906 at the Tübingen meeting of German Psychiatrists. In 1907 Alois published a scientific manuscript detailing his research about the disease. By 1910 the disease became known as Alzheimer’s Disease.
AD confirmed at autopsy with pathological diagnosis.
Brain imaging analysis such as PET, CT, and MRI developed to assist in diagnosing possible or probable AD.
Development and availability of cerebrospinal fluid (CSF) biomarker assessments to investigate pathological changes to assist in diagnosing possible or probable AD.
Blood-based biomarkers for phosphorylated tau demonstrate diagnostic accuracy and compare favorably with current corresponding CSF and neuroimaging biomarkers.
Plasma phospho-tau217 for demonstrates discriminative accuracy of Alzheimer’s disease vs. other neurodegenerative disorders with diagnostic precision equal to established diagnostic methods, including positron emission tomography (PET) imaging and cerebrospinal fluid biomarkers, both of which are expensive, invasive, and less accessible.
ALZpath is founded with the mission of transforming the Alzheimer’s disease ecosystem by innovating patient care, trials, and research through the integration of novel blood-based biomarkers, cognitive assessment tools, and care solutions.
Publications of Interest
Analytical and Clinical Assessment of Plasma Phospho-Tau Isoforms in Alzheimer's Disease (AD)
Neurology, 2023
Biofluid-based biomarkers for Alzheimer's disease-related pathologies: An update and synthesis of the literature
Alzheimer’s and Dementia, 2022
Moving fluid biomarkers for Alzheimer's disease from research tools to routine clinical diagnostics
Molecular Neurodegeneration, 2021
The validation status of blood biomarkers of amyloid and phospho-tau assessed with the 5-phase development framework for AD biomarkers
European Journal of Nuclear Medicine and Molecular Imaging, 2021